Your Pregnancy Help Organization and COVID-19
If you are a Heartbeat Affiliate, please click log in at the top of the page to view more materials! Additional materials will appear below for those current affiliates who are already logged in. Click here for more information about affiliating with Heartbeat International.
You can also get a recording of our webinar series Coronavirus and Your Pregnancy Help Organization for free by clicking here. Resources related to those webinars are also available on the Complimentary Materials page here.
The information in these articles is accurate as of the publication date of each one. We are working to keep our articles up-to-date as changes surrounding COVID-19 occur, and we encourage everyone to check the CDC, WHO and their local authorities as the situation is ever-evolving.
Displaying items by tag: sti
How Your Center Can Help Prevent Ebola's Spread

As the Ebola outbreak has spread from West Africa to isolated cases in parts of Europe and now the United States, there has been no shortage of panic and paranoia among Westerners—even those working in the health care fields.
Still, it is an established and repeated fact that Ebola's spread can be prevented simply by following proper safety procedures in a medical setting. An informational page on Ebola published at the World Health Organization's (WHO) website points to the sad reality of Ebola's largely preventable spread:
Health-care workers have frequently been infected while treating patients with suspected or confirmed EVD [Ebola Virus Disease]. This has occurred through close contact with patients when infection control precautions are not strictly practiced.1
As those involved in the life-saving work of pregnancy help in the medical setting, how can you protect yourself, your clinic, and your clients from this deadly virus?
The answer starts with educating yourself, your staff and volunteers, and your clients as to how Ebola spreads, which, again according to WHO, involves the following:
Ebola... spreads through human-to-human transmission via direct contact (through broken skin or mucous membranes) with the blood, secretions, organs or other bodily fluids of infected people, and with surfaces and materials (e.g. bedding, clothing) contaminated with these fluids.2
Consider the functions of your Pregnancy Help Medical Center or Clinic.
- Could you come into contact with any bodily fluid when handling a urine pregnancy test?
- What about collecting a specimen for STD/STI testing?
- Broken skin that can be exposed and contacted while conducting an ultrasound?
With these points of contact posing risks in light of the Ebola virus—in addition to several diseases that are much more likely to spread—make sure your center is paying special attention to policies such as Universal Precautions as defined by the Centers for Disease Control (CDC) and OSHA Regulations.
Under Universal Precautions, blood and certain body fluids of all patients are considered potentially infectious for HIV, (Hepatitis B), and other blood-borne pathogens. Universal Precautions involve the routine wearing of gloves, other protective clothing, hand washing, and such infection control measures that are designed to place a barrier between potentially infectious blood or body fluids and employees.3
For more information on how you can keep your center protected from the spread of viral infection, check out Heartbeat International's Medical Essentials for Pregnancy Help Organizations©.
1. "Ebola virus disease," World Health Organization, http://www.who.int/mediacentre/factsheets/fs103/en/ (accessed Oct. 17, 2014).
2. Ibid.
3. Medical Essentials for Pregnancy Help Organizations©, Heartbeat International, 2014, Part IV, page 4.
Transvaginal Sonogram: Is it Necessary in Your Medical Center?
by Audrey Stout, RN, RDMS, SoundView Imaging Partners
 |
In over ten years of educating abortion-vulnerable women on fetal development and abortion, I had seen many of these women experience a change of heart. Yet, for years, I also believed that if a woman was able to see her unborn child through ultrasound, many more would choose life. From the very beginning, we knew transvaginal ultrasound to be the best means of imaging a pregnancy in the early stages.
One objection we may not have anticipated was this: “We don’t want to do that, do we? What if the girls have not had a bath before coming?” Our medical team appropriately determined that we must “do that,” and then learned to perform both abdominal and transvaginal ultrasounds in order to provide pregnant women with services equal to the standard of care in the broader medical community.
Even with more than 600 pregnancy medical clinics offering medically indicated limited OB ultrasounds, there is still a lack of a common understanding for the necessity of transvaginal ultrasound in the pregnancy medical clinics, which bears itself out in resistance or hesitance to utilize this valuable resource. But transvaginal sonograms are absolutely necessary for pregnancy medical clinics.
The Importance of Transvaginal Ultrasound
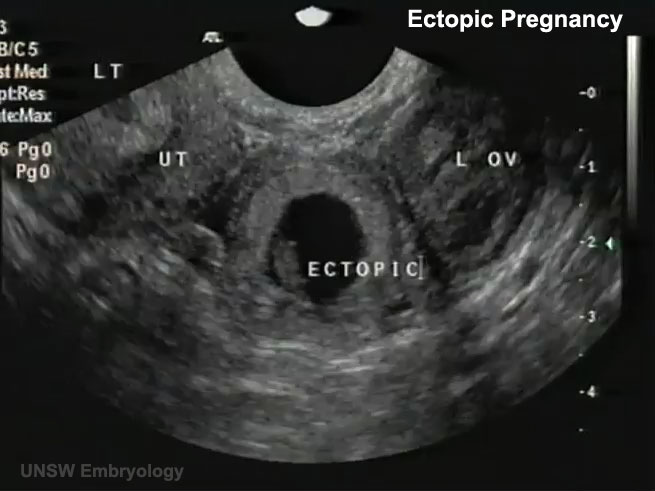
For early pregnancies, as well as women with a retroverted uterus or obesity, the use of transvaginal sonography is critical to determine the location of the pregnancy, since the child is tiny, and often not visible when scanning abdominally.
During a recent training involving around 60 scans, there were two patients for whom it was impossible to determine if there was a true gestational sac or pseudo sac of an ectopic pregnancy in the uterus by scanning abdominally. When the transvaginal probe was used, however, both ultrasounds revealed tiny embryos with beating hearts, measuring from 2-3 mm (25 mm=1 inch) in length alongside a yolk sac—diagnostic for an intrauterine pregnancy.
Apart from using the transvaginal probe in each of these cases, the patients would have needed both ectopic and miscarriage precautions, due to an inconclusive ultrasound. This would have required a follow-up scan, either at the PMC or with another physician, for serial hCG levels, in addition to another sonogram to rule out an ectopic pregnancy. This would have caused needless stress and concern, when the answers were available with a transvaginal scan. When a woman seriously considering abortion comes into a pregnancy clinic, we may only have one opportunity to see her and provide a life-affirming sonogram.
The three medical indications, for performing a limited OB sonogram in most PMCs according to the American Institution for Ultrasound in Medicine:
- To confirm the presence of an intrauterine pregnancy.
- To confirm cardiac activity.
- To estimate gestational age (EGA).
From the Textbook to the Pregnancy Medical Center
Every woman considering abortion needs this information to make a truly informed choice regarding her pregnancy. Using transvaginal sonography during the first trimester, one is much more likely to be able to answer the three questions listed above, and enable a woman to see the life of her unborn child in order to refute the idea that her child is just a mass of tissue.
PMCs typically see women in early pregnancy when they are most likely to have ectopic pregnancies, as most show symptoms between 7-8 weeks LMP. Since a ruptured ectopic pregnancy is life-threatening due to massive hemorrhage, every early sonogram must attempt to determine the location of the pregnancy. Ectopic pregnancy is the leading cause of first trimester maternal death, even though less than 9% of ectopics are actually visualized with a fetal pole on sonography because they are notoriously difficult to diagnose.
Skill in both transabdominal scanning and transvaginal scanning are necessary, as some ectopics or associated findings are visible with abdominal scanning, while most can only be visualized using transvaginal scanning. Transvaginal sonography also can uncover a rare condition known as “heterotopic pregnancy,” which is both intrauterine and ectopic, occurring at a rate of 1/30,000 in natural reproduction.
A recent article from MedPage Today discusses ectopic pregnancies and highlights the need for using transvaginal sonography. The article states:
Ectopic pregnancy occurs in up to 2.6% of all pregnancies and is the chief cause of first-trimester pregnancy-related mortality, accounting for up to 6% of maternal deaths. However, less than half of women with ectopic pregnancy have characteristic symptoms of abdominal pain and vaginal bleeding, which are more likely to indicate miscarriage.i
Further, ectopic pregnancy has been on the increase since 1970, when the Center for Disease Control began tracking this condition.
Key Factors to Keep in Mind
As those performing ultrasound services in the PMCs, adequate training is critical in order to gain skills in imaging the maternal anatomy, demonstrating with every sonogram that the pregnancy is intrauterine (IUP). If one does not possess these skills, it puts not only the woman who comes to you at-risk for losing her life, it also puts your PMC at legal risk of liability for harm. Thankfully, many women have been protected from life-threatening ectopic ruptures, due to the careful and skillful scanning of nurses and other medical personnel in PMCs.
Here are five tips to protect all involved by safely performing sonograms to the highest standard of medical care in your PMC:
- Attend a foundational didactic course for performing Limited OB Sonography in accordance to the Association of Women's Health, Obstetric and Neonatal Nurses Guidelines (AWHONN), e.g. the NIFLA course (NIFLA.org).
- Gain adequate hands-on training by an RDMS or physician skilled in performing OB sonograms to demonstrate competency in skills, both abdominally and transvaginally before performing sonograms without direct supervision. A minimum of 50 scans is strongly recommended for every sonographer, though for most, 60-75 may be needed. Documented competency is key to safety in scanning. Those skills should be assessed and refreshed on an annual basis.
- Follow a systematic scanning protocol, always beginning with an abdominal survey of the pelvis (including the adnexae and uterus) in two planes to identify the pregnancy location and get an idea of the gestational age.
- If with abdominal scan, one cannot clearly visualize anatomy (the vagina, cervix and contents of the uterus, i.e. gestational sac and fetal pole) with a high level of resolution to demonstrate an IUP, perform a transvaginal scan throughout the first trimester. When an IUP is not demonstrated, one must always suspect ectopic and provide precautions. Never assume it is too early.ii
- Consider sonography a life-long learning and skill journey, with excellence as the goal. For competency and skills growth, a sonographer should perform approximately 100-150 scans each year.
So, are transvaginal sonograms necessary in your PMC? Yes, yes, and yes.
Transvaginal sonograms safely provide sonography services and protect those served. In fact, sonographers with adequate training often happily admit, once they have acquired the skills, they very much prefer transvaginal scans because of the superior resolution and the fact that women are able to clearly see the image of their unborn child.
________________________________________
Audrey Stout, RN, RDMS, has a passion for the cause of life and began involvement with pregnancy centers in 1987. In 2000, she began instructing with NIFLA’s Limited OB Ultrasound Course and serves as National Nurse Manager Consultant for NIFLA as well. She has provided hands on trainings in sonography for PMCs medical personnel throughout the US, and is a founding partner with SoundView Imaging (SoundViewImaging.org). Audrey lives in Lexington, VA with her husband, Dave. They have three grown adopted children and one grandson.
Notes
i. Boyles, S. Transvaginal Ultrasound Best to Find Ectopic Pregnancy. April 23, 2013. Medpage Today. Accessed June 25, 2013 from: http://www.medpagetoday.com/OBGYN/Pregnancy/38638.
ii. Bourgon, D., Lin, E., Ectopic Pregnancy Imaging. April 12, 2011. Medscape. Accessed June 28, 2013 from: http://emedicine.medscape.com/article/403062-overview.