Displaying items by tag: pregnancy
Pregnancy Help Appreciation Week Videos

. . . . .
Bernadette Tasy, Alliance Defending Freedom
Amy Ford, Embrace Grace
Jeanne Mancini
Kristan Watson, Students for Life
Robyn Chambers - Focus on the Family
Bernadette Tasy - Alliance Defending Freedom
Melissa Ohden - Abortion Survivors Network
Eric Scheidler - Pro-Life Action League
Jeanne Mancini - March for Life
Sarah Gabel Seifert - EveryLife
Kristan Hawkins - Students for Life
. . . . .
Like these? Check out videos from past Pregnancy Help Appreciation Weeks. You are loved. And the work you do is admired.

And don't forget to check out the deals of the day and share the love on social media!
Pregnancy Help Appreciation Week - November 11-15, 2024
What is Pregnancy Help Appreciation Week?
Pregnancy Help Appreciation Week was designed by Heartbeat International to honor those working within the pregnancy help movement. Through their work, women and men receive the compassionate support they need when facing a life-changing decision. They walk alongside families throughout the pregnancy and beyond, blessing them with pregnancy tests, emotional support, ultrasounds, parenting classes, and so much more at no cost.
From volunteers to executive directors, nurses to receptionists, each person working in a pregnancy help organization has been gifted with the passion to advance the culture of LIFE! And for that, we thank you!
This year's Pregnancy Help Appreciation Week is November 11-15, 2024.
How you can thank a Pregnancy Help Foot Soldier:
- Pray. The emotional energy given by those who work in the pregnancy help movement is extreme. They give of themselves daily. Pray for spiritual refreshment for those who go into the center today.
- Volunteer. Connect with your local pregnancy help organization and see what their needs are. You may have just the right skills to fill a need.
- Donate items. Call your local pregnancy help organization and ask them what items they need to bless a new mother (such as diapers or maternity clothes) and start collecting. Not only will you bless a center, you will bless multiple families as well.
- Give. Without the generous donations of those within the community, pregnancy centers would not be able to provide their services for free.
- Share the love. Share the good work of the pregnancy help community with your social networks. Don't know what to post? Like Heartbeat International on Facebook and/or Instagram and you'll find plenty to share!
If you haven't heard of Pregnancy Help Appreciation Week before, you should expect special deals, thank-you messages, and extra prayers this week.
Plus! We'll be holding a drawing at the end of the week where one lucky winner will get a fun gift basket from us at Heartbeat!
. . . . .
Shareables
Click on each image to view the full-sized version. Then, save it to your device and share on Facebook, Instagram, or tweet and show your love for the pregnancy help movement using the hashtag #ThankAPregnancyCenter
. . . . .
Friday's Deal of the Day = ALL Deals + Free Resources!
We're bringing back all the week's deals for one last hurrah! Plus, there are a few Free Resources to check out. After today, you won't see deals like this again until *next* November.
Let's recap—today only you get...
$5 Monday Deals:
Changing Clients- Shifting Focus (housing)
Discussing the Adoption Option in a Post-Roe America
Onboarding Board Members for Successful Service
Postpartum Depression
Protecting Minors from Trans On Demand Interventions
Sex Trafficking & Abortion
The Truth About Backstreet Abortion
$2 Tuesday Deals:
Opioids and Pregnancy
How to Identify and Use a Media "Hit" Piece
Surviving Christmas: Healing Resident Trauma During the Holidays
Speaking at Churches in a Post-Roe World
Healthy Boundaries in Ministry
Abortion's Long-Term Negative Impact on Men
Healing from Medication Abortion Trauma
Special Considerations of Healing from Diagnosis Abortions
50% off Wednesday Deals:
Identifying Fake Client
Advancement Bootcamp
How to Identifying and Assist Victims of Human Trafficking
75% off Thursday Deal:
From an archive of our Conference recordings of the past 5 years, get the bundle on a topic of your choice for 75% off.
*PLUS*
Free Resources
At the Heart of What it Takes to go Mobile
by Michele Chadwick, Director of Operations, ICU Mobile
 Heartbeat's Betty McDowell gave an encouraging message in her presentation at the 2014 Heartbeat International Conference, which came down to a single phrase: I see you. The God of the universe acknowledges and recognizes you. You are valid.
Heartbeat's Betty McDowell gave an encouraging message in her presentation at the 2014 Heartbeat International Conference, which came down to a single phrase: I see you. The God of the universe acknowledges and recognizes you. You are valid.
At ICU Mobile, our name and mobile ultrasound ministry (ICU, think "I See You") was born out of a call to proactively reach out to help mothers see their babies in the womb, identifying that every life is valid—sometimes for the first time in a mother's heart.
Revealing and affirming life is at the heart of all our ministries, serving a vital, essential role in life-affirming work. When a pregnancy center provides medical ultrasound imaging, its representatives affirm that the act of visibly revealing life is essential to the ability to fully inform a pregnant mother of the life she carries.
Going mobile medically brings this vital life-imaging service to mothers outside of the center. At ICU Mobile, we believe that at the heart of an accomplished mobile medical clinic, as in the pregnancy center, is a commitment to offer services with faith, wisdom, and experience as our guide. We are committed to standing strongly on the strategic operating principle of extending the reach of our services for women into the –community—in the community of others.
A mobile medical clinic, when operating well, is a tool with the capability of joining a community together under the umbrella of life, drawing pregnancy resource centers together with the church and other community and organizational resources, in support of each other in the service of women.
Key factors that help encourage this united front include neutral branding, a process to provide a full continuum of care for the client, operating from each other's strengths through shared service models, and encouraging good stewardship through shared resources.
 Pregnancy help expert Kirk Walden, in his book, "The Wall" (and who also presented at the Heartbeat Conference!) makes the case for uniting the community to serve women. He asks the question, "What happens if we're the first choice?" The "we" in this question is key. The "we" is all of us working together to be a mother's first choice. A mobile medical clinic can be the "vehicle" (no pun intended) for building this unity.
Pregnancy help expert Kirk Walden, in his book, "The Wall" (and who also presented at the Heartbeat Conference!) makes the case for uniting the community to serve women. He asks the question, "What happens if we're the first choice?" The "we" in this question is key. The "we" is all of us working together to be a mother's first choice. A mobile medical clinic can be the "vehicle" (no pun intended) for building this unity.
Mobile operations in joining others together can become one of the most effective ways to reach abortion-minded women. Mobile services provide an effective way to expand your reach without having to build a satellite office, expand internally, or require more space, and it allows a center the flexibility to move to locations to adjust to demographic changes and population shifts.
Further, going mobile avoids the issue of no-show appointments at your center, as well as helping to balance the number of clients seeking social support services and those seeking medical services. Going mobile alleviates the expense of renovation or expansion of services in your center, while providing opportunities to build network supports with other pregnancy help organizations in the community surrounding the center.
Each of these considerations factor into the thought process of going mobile in a community.
When considering the possibility of adding a mobile medical clinic, it is first important—as with adding any medical service—to recognize the seriousness of the endeavor and requires the highest level of commitment to a professional quality medical experience for the client, as it is visible and the first contact with a mother.
Equally important for an organization to note is that going mobile is a unique approach that influences how a center operates, affecting the procedural processes that are needed to accommodate a moving center. A board, leaders, staff, and the connected community must pray and seek wisdom and recognition of the call to serve in this mission capacity.
We recommend you seek others who already operate a mobile medical clinic to learn about effective methods of operation, strategies that work, and the significance of working together in community to serve. It is God who builds these mobile communities, so it will be God who lays the possibility and provides the opportunity for success.
As Kirk Walden asked at the Heartbeat Conference, "What can we do to join hands?" Mobile done in community with others will join hands, and as we are blessed to say at ICU Mobile, it joins hands for little feet.
Here are some practical questions and steps toward adding mobile services:
- Do you have a need to reach women in multiple locations who would benefit from the ability to change locations daily?
- Is your board and staff ready to take a logistically challenging step that would involve a comprehensive team effort?
- Contact ICU mobile and ask questions that would be important for you to consider when incorporating a new program.
- Once the board has the buy-in, meet with top donors to survey their interest in the project.
- Investigate friends and "influencers" on local college campuses to assess their interest.
Shelf Help: Tiny Blue Lines
 Endorsed by Heartbeat International President Peggy Hartshorn, Tiny Blue Lines is a young mother's story that started the day she saw two tiny blue lines after taking a pregnancy test.
Endorsed by Heartbeat International President Peggy Hartshorn, Tiny Blue Lines is a young mother's story that started the day she saw two tiny blue lines after taking a pregnancy test.
"Tiny Blue Lines is a triumph of faith and courage, and a treasury of resources for all who choose life," Peggy says in her endorsement.
The book's author, Chaunie Marie Brusie is a strong Christian pro-life advocate whose personal journey through pregnancy and young motherhood as a college student is mixed with other, similar stories of courageous women who took on the challenge and difficulties of welcoming new life.
To find out more, visit Tiny Blue Lines at TinyBlueLines.com
6 Effective Ways to Mentor a Teen Parent
 |
With the help of our local pregnancy center, I established a list of what was most important to keep in mind when coming alongside a teen parent.
Where do you start this process? Once she is committed to life, begin to expose her to six areas that may be unfamiliar to most teenagers:
- Social Services (with a twist)
- Spiritual Encouragement
- Education Options
- Community Awareness
- Care and Concern
- Support Emphasis
Wrapping around a teen parent will involve guiding wisdom, generous amounts of spiritual insight, as well as an understanding of the vast array of social services and guidance in community awareness… Oh, and a lot of care.
The hope is to address and meet this young mother’s needs by utilizing all these areas of service that already exist around her.
Social Services
Help mom jump through the hoops of social services. Bring the social services to her. Monthly group meetings highlighting local, state, and federal resources benefit your clients, as well as bringing a vast array of networking opportunities your center’s way. Imagine for a moment you’re a teenager, trying to sort through medical papers and legal jargon. Help mom see the benefits to these services by empowering her to make choices. Start with identifying the services available to her. Sort through them, and piece together those with the best-suited benefits.
If your center offers a packet of resources available in your area, that’s a great start… But, what if you take it one step further?
What if you offer to go through that packet of information with this client? What if you arrange a follow-up, educational, session to equip her with all the information she needs?
The Twist… Give Back!
The twist to Social Services is training your clients to give back. When we eat too much, we get full. Too much candy causes tooth decay and tummy aches. Ask any 5-year-old after Halloween. Too much of anything generally leads to trouble.
Giving back is a powerful teaching tool. If we dismiss giving back as an educational-teaching tool, we completely miss out on the blessing that comes with giving. There is growth and maturity that transpires in giving. There is something powerful in saying, "I gave to someone else. I was useful, and I helped."
We only need to remember a time when the Lord used us to help another, and how satisfying it was to have been used. The principle of giving transcends understanding. Teach your teen clients to give back now and they will reap the benefits.
Spiritual Encouragement
To mentor someone means to come alongside them as a wise, trusted guide. How do you mentor a teen mom or dad? Gently, by the hand. You cannot force a teenager to do anything. A shepherd (or a mentor) diligently looks after his and quickly responds to any lost lambs. He gently curbs them back to the flock and leads them (Matthew 18:10-14).
Ultimately, we must remember your client is a teenager, a child in her own right. She does not need our judgment. She needs our love and support. Teen parents need to know they can be forgiven. They may or may not know the acts they have committed were sinful, but they will most likely feel the shame others place upon them.
Teens will not listen to your words with as much attention as they will watch your actions. Moving in love towards mom will motivate change quicker than mere words. If your actions toward here are loving, she will not expect you to be "up" on the latest texting fad or care that you don’t understand all the functions on your Smartphone.
Concern can be felt when you enter the room. How is your presence perceived? How would she feel when you entered the room? Would she feel judgment or embrace?
Educational Options
Your teen parent will need help exploring her educational options. Make your center staff and volunteers aware of local high school programs. A director who’s savvy in these areas will be able to make options available for clients.
Contact your local High School and request a collaboration meeting, looking for various networking opportunity such a meeting would present. Initially, there may not be a warm reception to this idea, depending on the department's worldview. But go into this meeting prepared, with your agenda in hand.
What questions do teen parents ask regarding education? Are there established plans in place for teen parents? What educational options do teen dads have, if any? How can both entities—the school and your center—work together for the betterment of the teens?
Are there resources you can provide, or ways you can both partner together to encourage academic success during the teen parents’ high school and college years?
Even if these meetings are not pleasant, keep in mind that an educational advocate is needed for teens in several arenas. Your center represents that for teen parents!
Are there other resources centers can provide for additional support? Creatively structure a child-free study hall time, manned with knowledgeable volunteers who are willing to assist with homework. You can also consider dedicating one night a week to a homework-help hotline for teen parents. Reaching out in the educational realm will broaden your scope, and has the potential to draw more teens from the community.
Community Awareness
I am currently working with a creative bunch to lead a single mom's ministry within our church. Our reoccurring discussion is, "How do we advertise this group and offer support to the community and families at-large without isolating or offending single-parent households?"
We want to be sensitive so they do not feel put forth for judgment. Our goal is to wrap love around them and provide them with unique services. I am learning a great deal about my approach to these women through a friend who is also a single parent. Single moms do not necessarily choose this option. It's a lot of tough work. Many are alone, making hope out of less-than-hopeful situations.
As a church, we do not want to error in our approach to love them. Since I am not a single parent, it takes effort on my part to more accurately relate to and understand single parents. I must educate myself through resources and other women. That's exactly it! Awareness does take work!
Are you and your center willing to exert yourselves to really get to know these young moms? Are you willing to walk in her shoes in full view of both Christian and Non-Christian communities made up of judges who focus only on her sin and mistakes?
Are you willing to advocate for them?
One of the teenage moms I interviewed expressed through tears the shame and judgment she experienced firsthand from her school nurse. The hurtful words expressed were written across this young woman's face and proven in her tears.
How does your center promote a healthy outlook for teen parents in your community? First, it begin with you, your staff, and volunteers by renewing your commitment to teen parents. Activate this commitment by hosting focused annual workshops and trainings on community awareness for local churches, the community at-large (i.e., local public libraries), as well as local school boards.
Continual training and awareness-raising actively pursues the hearts of these young women and educate others on ways to support them. Providing trainings for the community and for churches exposes the teen parents' struggles and the reality of these situations. It may also be useful to attract donors for your cause.
Go with the hearts of these young mothers in mind, and anxiously wait upon the Lord to provide wisdom, acceptance, love, and the potential of new funding.
Care & Concern
View the development of care and concern as a flower. Every flower starts with a seed. When properly planted, growth is likely to occur.
Fostering care and concern starts the moment the client enters your building. Offer the teen parent support, resources, and supplies. Pray this seedling germinates into deep roots once authentic care, legitimate concern, and plenty of prayer permeate her life.
When mom knows you actually care about her, the relationship you offer can grow. Research has a lot to say about the client/volunteer relationship (or whoever works closest to her), suggesting the client/volunteer relationship can be more important than anything discussed. Use your relationship with mom as a training model. Chances are, she may have poor interpersonal skills and her relationships may need major repairs. The client/volunteer bond can be used as a guide for her to cultivate healthier friendships with others.
Growth brings change, and we know that true change only comes from the Holy Spirit. Pray she fixes her mind upon Him (Hebrews 12:2), and He changes old mindsets (Ephesians 4:20-24). He can make all things new!
Support Emphasis
Offer to help put a support plan in place. Who are her current support people? These are the dominant figures involved in her life. Creating a support plan allows you to know the valuable people in her life. It also gives her the opportunity to establish a list of people to access. Good or bad, this list will quickly tell you a lot about her current status and situation.
Does she have people who support her? What roles do these people serve? Where is she lacking in support? What needs still exist? A support plan provides her with needed resources, including people resources.
Bringing it Home
When mentoring teen parents, take an honest evaluation of the services your center currently provides. Consider restructuring or increasing your existing services to fully experience success. Think outside the box when given the opportunity to do life with teens.
All the while, keep in mind the truth that our God is not limited by your resources or skills. He will be blessed as you work for "the least of these" (Matthew 25:40). Thank you for serving!
Rebecca Dawson is author of "Help! I'm a Mom-To-Be!", which gives a comprehensive view for creating a support plan and offers greater detail and application on these discussed topics.
Transvaginal Sonogram: Is it Necessary in Your Medical Center?
by Audrey Stout, RN, RDMS, SoundView Imaging Partners
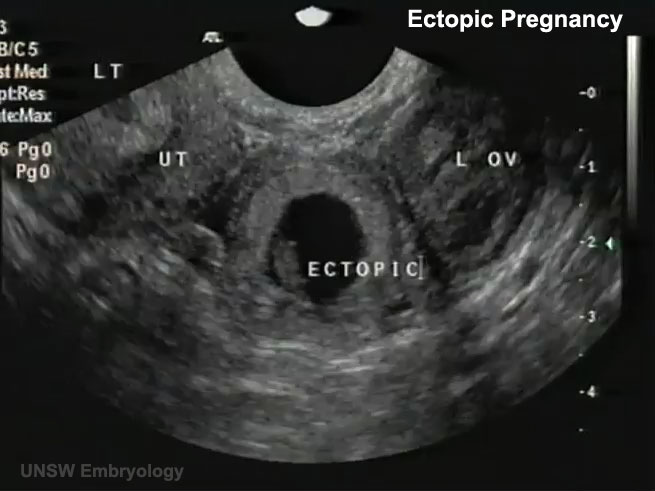 |
In over ten years of educating abortion-vulnerable women on fetal development and abortion, I had seen many of these women experience a change of heart. Yet, for years, I also believed that if a woman was able to see her unborn child through ultrasound, many more would choose life. From the very beginning, we knew transvaginal ultrasound to be the best means of imaging a pregnancy in the early stages.
One objection we may not have anticipated was this: “We don’t want to do that, do we? What if the girls have not had a bath before coming?” Our medical team appropriately determined that we must “do that,” and then learned to perform both abdominal and transvaginal ultrasounds in order to provide pregnant women with services equal to the standard of care in the broader medical community.
Even with more than 600 pregnancy medical clinics offering medically indicated limited OB ultrasounds, there is still a lack of a common understanding for the necessity of transvaginal ultrasound in the pregnancy medical clinics, which bears itself out in resistance or hesitance to utilize this valuable resource. But transvaginal sonograms are absolutely necessary for pregnancy medical clinics.
The Importance of Transvaginal Ultrasound
For early pregnancies, as well as women with a retroverted uterus or obesity, the use of transvaginal sonography is critical to determine the location of the pregnancy, since the child is tiny, and often not visible when scanning abdominally.
During a recent training involving around 60 scans, there were two patients for whom it was impossible to determine if there was a true gestational sac or pseudo sac of an ectopic pregnancy in the uterus by scanning abdominally. When the transvaginal probe was used, however, both ultrasounds revealed tiny embryos with beating hearts, measuring from 2-3 mm (25 mm=1 inch) in length alongside a yolk sac—diagnostic for an intrauterine pregnancy.
Apart from using the transvaginal probe in each of these cases, the patients would have needed both ectopic and miscarriage precautions, due to an inconclusive ultrasound. This would have required a follow-up scan, either at the PMC or with another physician, for serial hCG levels, in addition to another sonogram to rule out an ectopic pregnancy. This would have caused needless stress and concern, when the answers were available with a transvaginal scan. When a woman seriously considering abortion comes into a pregnancy clinic, we may only have one opportunity to see her and provide a life-affirming sonogram.
The three medical indications, for performing a limited OB sonogram in most PMCs according to the American Institution for Ultrasound in Medicine:
- To confirm the presence of an intrauterine pregnancy.
- To confirm cardiac activity.
- To estimate gestational age (EGA).
From the Textbook to the Pregnancy Medical Center
Every woman considering abortion needs this information to make a truly informed choice regarding her pregnancy. Using transvaginal sonography during the first trimester, one is much more likely to be able to answer the three questions listed above, and enable a woman to see the life of her unborn child in order to refute the idea that her child is just a mass of tissue.
PMCs typically see women in early pregnancy when they are most likely to have ectopic pregnancies, as most show symptoms between 7-8 weeks LMP. Since a ruptured ectopic pregnancy is life-threatening due to massive hemorrhage, every early sonogram must attempt to determine the location of the pregnancy. Ectopic pregnancy is the leading cause of first trimester maternal death, even though less than 9% of ectopics are actually visualized with a fetal pole on sonography because they are notoriously difficult to diagnose.
Skill in both transabdominal scanning and transvaginal scanning are necessary, as some ectopics or associated findings are visible with abdominal scanning, while most can only be visualized using transvaginal scanning. Transvaginal sonography also can uncover a rare condition known as “heterotopic pregnancy,” which is both intrauterine and ectopic, occurring at a rate of 1/30,000 in natural reproduction.
A recent article from MedPage Today discusses ectopic pregnancies and highlights the need for using transvaginal sonography. The article states:
Ectopic pregnancy occurs in up to 2.6% of all pregnancies and is the chief cause of first-trimester pregnancy-related mortality, accounting for up to 6% of maternal deaths. However, less than half of women with ectopic pregnancy have characteristic symptoms of abdominal pain and vaginal bleeding, which are more likely to indicate miscarriage.i
Further, ectopic pregnancy has been on the increase since 1970, when the Center for Disease Control began tracking this condition.
Key Factors to Keep in Mind
As those performing ultrasound services in the PMCs, adequate training is critical in order to gain skills in imaging the maternal anatomy, demonstrating with every sonogram that the pregnancy is intrauterine (IUP). If one does not possess these skills, it puts not only the woman who comes to you at-risk for losing her life, it also puts your PMC at legal risk of liability for harm. Thankfully, many women have been protected from life-threatening ectopic ruptures, due to the careful and skillful scanning of nurses and other medical personnel in PMCs.
Here are five tips to protect all involved by safely performing sonograms to the highest standard of medical care in your PMC:
- Attend a foundational didactic course for performing Limited OB Sonography in accordance to the Association of Women's Health, Obstetric and Neonatal Nurses Guidelines (AWHONN), e.g. the NIFLA course (NIFLA.org).
- Gain adequate hands-on training by an RDMS or physician skilled in performing OB sonograms to demonstrate competency in skills, both abdominally and transvaginally before performing sonograms without direct supervision. A minimum of 50 scans is strongly recommended for every sonographer, though for most, 60-75 may be needed. Documented competency is key to safety in scanning. Those skills should be assessed and refreshed on an annual basis.
- Follow a systematic scanning protocol, always beginning with an abdominal survey of the pelvis (including the adnexae and uterus) in two planes to identify the pregnancy location and get an idea of the gestational age.
- If with abdominal scan, one cannot clearly visualize anatomy (the vagina, cervix and contents of the uterus, i.e. gestational sac and fetal pole) with a high level of resolution to demonstrate an IUP, perform a transvaginal scan throughout the first trimester. When an IUP is not demonstrated, one must always suspect ectopic and provide precautions. Never assume it is too early.ii
- Consider sonography a life-long learning and skill journey, with excellence as the goal. For competency and skills growth, a sonographer should perform approximately 100-150 scans each year.
So, are transvaginal sonograms necessary in your PMC? Yes, yes, and yes.
Transvaginal sonograms safely provide sonography services and protect those served. In fact, sonographers with adequate training often happily admit, once they have acquired the skills, they very much prefer transvaginal scans because of the superior resolution and the fact that women are able to clearly see the image of their unborn child.
________________________________________
Audrey Stout, RN, RDMS, has a passion for the cause of life and began involvement with pregnancy centers in 1987. In 2000, she began instructing with NIFLA’s Limited OB Ultrasound Course and serves as National Nurse Manager Consultant for NIFLA as well. She has provided hands on trainings in sonography for PMCs medical personnel throughout the US, and is a founding partner with SoundView Imaging (SoundViewImaging.org). Audrey lives in Lexington, VA with her husband, Dave. They have three grown adopted children and one grandson.
Notes
i. Boyles, S. Transvaginal Ultrasound Best to Find Ectopic Pregnancy. April 23, 2013. Medpage Today. Accessed June 25, 2013 from: http://www.medpagetoday.com/OBGYN/Pregnancy/38638.
ii. Bourgon, D., Lin, E., Ectopic Pregnancy Imaging. April 12, 2011. Medscape. Accessed June 28, 2013 from: http://emedicine.medscape.com/article/403062-overview.
Response to CDC Report: Decline in State Teen Birth Rates by Race and Hispanic Origin
 |
This article was originally written by the Medical Institute for Sexual Health, received July 1, 2013. It is reprinted as written in its entirety with permission.
In May 2013, the CDC released the report Decline in State Teen Birth Rates by Race and Hispanic Origin.1 This report includes four important findings. First, the teen birth rates fell by at least 15% for all but two states during 2007 – 2011. In fact, seven of these states recorded a decrease of about 30% or more.1
Second, this decline in teen birth rates was most rapid in Hispanic teenagers who achieved a 34% reduction, followed by non-Hispanic Blacks at 24% and non-Hispanic white teens at 20%.1
Third, the recorded long-term difference between teen birth rates for non-Hispanic blacks and Hispanic teenagers had gradually disappeared over five years of follow-up data from 2007 – 2011, and the rates had become virtually identical for both groups in 2011, the most current year for which data is available.1,2
Fourth, the rates for Hispanic teens fell about 40% or more in 22 states and the District of Columbia.1 In all, rates for Hispanic teens decreased by at least 30% in 37 states and DC.1
Although this decrease has been attributed to an increased use of contraception (long acting reversible contraceptives (LARCs), oral contraceptive pills, and condoms) among teenagers;3 the number of teens who have initiated sexual intercourse or are currently sexually active has been on the decline.4 This trend has also been a contributory factor in decreasing teen pregnancies and consequently teen births. However; the rates of sexually transmitted infections have been on the rise among sexually active teenagers and young adults aged 15 – 24 years.5
Even with the record decline among all populations of teens; especially in minority populations, the work is not yet done in making sure this trend is sustained among teens of all ethnic groups. Focusing on sexual health education, character training, and parenting education at the community level are all initiatives that could address different needs of various populations within the US. Currently, the Medical Institute offers training to health educators and community liaisons to teach these topics to parents in a wide range of communities across the US.
Surveys continue to show that parents are very influential in the sexual decision making of their children but that parents are frequently unaware of this influence.5 Therefore, it is important for parents to be prepared to discuss these topics with their children. Increasing the involvement of parents in the sexual and character education of their children offers the opportunity to capitalize on the unique position of influence that parents hold and to deliver the message in an individualized, culturally-appropriate way.
We cannot underestimate the role of a number of social factors that influence the sexual behavior of teenagers. However, evaluation studies have shown a common thread in the positive effect of parental communication and connectedness in delaying sexual initiation and helping young people make healthy sexual decisions.6
The decline in teen birth rates is a welcome development. However, the STI rates among this population have been increasing. Working towards a reduction in the rates of other attendant negative outcomes of early sexual initiation such as sexually transmitted diseases and emotional consequences is also critical. Consequently, a risk avoidance prevention message continues to take priority in achieving this goal. Avoiding all risky behaviors is the most reliable way to prevent the myriad of adverse outcomes associated with such behaviors. By emphasizing risk avoidance messages; parents, parenting adults and educators can guide youth towards making the healthiest decisions and leading productive lives.
About Medical Institute for Sexual Health
The mission of the Medical Institute for Sexual Health is “To empower safe, healthy living by communicating objective and scientific sexual health information.” MI is focusing on five initiatives: Parent Education, Adolescent and College Education, Sex in Media, Medical Accuracy, and Medical Education. These initiatives will facilitate access to medically accurate, evidence-based sexual health information.” The Medical Institute offers a wealth of information and resources relating to sexual health. For additional information, visit https://www.medinstitute.org/.
References:
- Hamilton BE, Mathews TJ, Ventura SJ. Declines in state teen birth rates by race and Hispanic origin. NCHS data brief, no 123. Hyattsville, MD: National Center for Health Statistics. 2013. Available at: http://www.cdc.gov/nchs/data/databriefs/db123.htm . Accessed June 28, 2013.
- Hamilton BE, Ventura SJ. Birth rates for U.S. teenagers reach historic lows for all age and ethnic groups. NCHS data brief, no 89. Hyattsville, MD: National Center for Health Statistics. 2012. Available at: http://www.cdc.gov/nchs/data/databriefs/db89.htm . Accessed June 28, 2013.
- Martinez G, Copen CE, Abma JC. Teenagers in the United States: Sexual activity, contraceptive use, and childbearing, 2006–2010 National Survey of Family Growth. National Center for Health Statistics. Vital Health Stat 23(31). 2011.
- CDC. Youth Risk Behavior Surveillance—United States, 2011. MMWR. 2012;61(No. SS-4). Available at: http://www.cdc.gov/mmwr/pdf/ss/ss6104.pdf . Accessed June 28, 2013.
- Satterwhite CL, et al. Sexually transmitted infections among U.S. women and men: prevalence and incidence estimates, 2008. Sex Transm Dis 2013; 40(3): 187-193.
- Albert, B. (2012). With One Voice 2012: America’s Adults and Teens sound Off About Teen Pregnancy. Washington, DC: The National Campaign to Prevent Teen and Unplanned Pregnancy. Available at: http://www.thenationalcampaign.org/wov/ . Accessed June 28, 2013.
- Markham CM, Lormand D, Gloppen KM, Peskin MF, Flores B, Low B, House LD. Connectedness as a predictor of sexual and reproductive health outcomes for youth. J Adolesc Health.2010; 46(3):S23-S41.
Prepping for a Healthy Pregnancy
The following information is found at the CDC site:
Not all birth defects can be prevented. But a woman can increase her own chances of having a healthy baby by managing health conditions and adopting healthy behaviors before becoming pregnant. This is important because many birth defects happen very early during pregnancy, sometimes before a woman even knows she is pregnant.
 Here are 10 steps a woman can take to get ready for a healthy pregnancy:
Here are 10 steps a woman can take to get ready for a healthy pregnancy:
- Take 400 micrograms (mcg) of folic acid every day. Folic acid is a B vitamin. If a woman has enough folic acid in her body at least 1 month before and during pregnancy, it can help prevent major birth defects of the baby’s brain and spine.
- Don't drink alcohol at any time during pregnancy. When a woman drinks alcohol, so does her unborn baby. Alcohol in the woman’s blood passes through the placenta to her baby through the umbilical cord. There is no known safe amount of alcohol to drink while pregnant. There also is no safe time during pregnancy to drink and no safe kind of alcohol. Drinking alcohol during pregnancy can cause a baby to be born with a birth defect.
- Don’t smoke. The dangers of smoking during pregnancy include premature birth, certain birth defects (cleft lip or cleft palate), and infant death. Even being around cigarette smoke puts a woman and her unborn baby at risk for problems. Quitting smoking before getting pregnant is best. But for a woman who is already pregnant, quitting as early as possible can still help protect against some health problems for the baby, such as low birth weight. It’s never too late to quit smoking.
- Don’t use “street” drugs. A woman who uses illegal—or “street”—drugs during pregnancy can have a baby who is born premature with low birth weight, or has other health problems, such as birth defects. A woman who uses cocaine while pregnant is more likely to have a baby with birth defects of the arms, legs, urinary system, and heart. Other drugs, such as marijuana and ecstasy, also can cause birth defects among babies.
It also is important that a woman not use "street" drugs after she gives birth, because such drugs can be passed through breast milk to her baby and can affect the baby’s growth and development. If you use "street" drugs, talk with your doctor about quitting before you get pregnant. - Talk to a health care provider about taking any medications. Taking certain medications during pregnancy can cause serious birth defects, but the safety of many medications taken by pregnant women has been difficult to determine. If you are pregnant or planning a pregnancy, you should not stop taking medications you need or begin taking new medications without first talking with your doctor. This includes prescription and over-the-counter medications, as well as dietary or herbal products.
- Prevent infections. Some infections that a woman can get during pregnancy can be harmful to the unborn baby. Learn how to help prevent infections.
- Talk to your doctor about vaccinations (shots). Many vaccinations are safe and recommended during pregnancy, but some are not. Having the right vaccinations at the right time can help keep a woman and her baby healthy.
- Keep diabetes under control. Poor control of diabetes during pregnancy increases the chances for birth defects and other problems for the baby. It can also cause serious complications for the woman. Proper healthcare before and during pregnancy can help prevent birth defects and other poor outcomes.
- Reach and maintain a healthy weight. A woman who is obese (a body mass index of 30 or higher) before pregnancy is at a higher risk for complications during pregnancy. Obesity in the woman also increases the risk of several serious birth defects for the baby. If you are overweight or obese, talk with your doctor about ways to reach a healthy weight before you get pregnant.
- See a health care professional regularly. A woman should be sure to see her doctor when planning a pregnancy and start prenatal care as soon as she thinks that she is pregnant. It is important to see the doctor regularly throughout pregnancy, so a woman should keep all her prenatal care appointments.
 Six tips from the American Pregnancy Association:
Six tips from the American Pregnancy Association:
Awareness and education are the first steps to preventing birth defects. The immediate step following awareness and education is taking action. There are a number of things you can do to increase the probability of having a healthy pregnancy and a healthy baby. Some are more challenging than others because they require that you break habits, but it is worth your effort.
Here are a variety of tips you can use to prevent birth defects as you contemplate starting or adding to your family:
Tip 1. The first and foremost tip is maintaining preconception health; eating well balanced and nutritional meals, and taking a multivitamin daily that includes the recommended 400 mcg of folic acid.
Tip 2. If you are sexually active and pregnancy is a possibility, make sure you take a multivitamin daily which includes the recommended 400 mcg of folic acid and other essential B vitamins.
Tip 3. Avoid all activities that could potentially lead to birth defects including alcohol, tobacco, illicit drugs, and caffeine.
Tip 4. Seek an annual gynecological and wellness exam.
Tip 5. Obtain genetic counseling and birth defect screening, particularly if you have any family history of birth defects or if you are 35 years of age or older.
Tip 6. Help your family or friends who might be considering parenthood by informing them that January is Birth Defects Prevention Month. You can send an e-mail and link to this page to everyone in your address book.”
More recommendations from the CDC:
-
Premature Birth: Important growth and development occur throughout pregnancy – all the way through the final months and weeks. Babies born three or more weeks earlier than their due date have greater risk of serious disability or even death. Learn the warning signs and how to prevent a premature birth.
-
Folic Acid: Folic acid is a B vitamin that can help prevent major birth defects. Take a vitamin with 400 micrograms (mcg) of folic acid every day, before and during pregnancy.
- Smoking during pregnancy is the single most preventable cause of illness and death among mothers and infants. Learn more about the dangers of smoking and find help to quit.
- Alcohol: When you drink alcohol, so does your unborn baby. There is no known safe amount of alcohol to drink while pregnant.
- Vaccinations: Talk to your doctor about vaccinations (shots). Many are safe and recommended during pregnancy, but some are not. Having the right vaccinations at the right time can help keep you and your baby healthy.
- Flu and Pregnancy: If you're pregnant, a flu shot is your best protection against serious illness from the flu. A flu shot can protect pregnant women, their unborn babies, and even their babies after birth.
- Infections: You won’t always know if you have an infection—sometimes you won’t even feel sick. Learn how to help prevent infections that could harm your unborn baby.
- HIV: If you are pregnant or are thinking about becoming pregnant, get a test for HIV as soon as possible and encourage your partner to get tested as well. If you have HIV and you are pregnant, there is a lot you can do to keep yourself healthy and not give HIV to your baby.
- West Nile Virus: Take steps to reduce your risk for West Nile virus and other mosquito-borne infections.
- Diabetes: Poor control of diabetes during pregnancy increases the chance for birth defects and other problems for your baby. It can cause serious complications for you, too.
- High Blood Pressure: Existing high blood pressure can increase your risk of problems during pregnancy.
- Medications: Taking certain medications during pregnancy might cause serious birth defects for your baby. Talk to your doctor or pharmacist about any medications you are taking. These include prescription and over-the-counter medications and dietary or herbal supplements.
- Environmental and Workplace Exposures: Some workplace hazards can affect the health of your unborn baby. Learn how to prevent certain workplace hazards. If you are worried about a specific substance, please click here.
- Unborn Babies Exposed to Radiation: If you think you might have been exposed to radiation, talk with your doctor.
- Pediatric Environmental Health Specialty Units:
A network of experts in children's environmental health.
Tips to Get a Fetal Heart Beat
By Kimela Hardy, MA, RT(R), RDMS
Available literature states the fetal heart beat begins its lifelong work at approximately six weeks, and depending on the sonographer’s skills, ultrasound system, and maternal body habitus, the heart beating may be visualized at this time. There are several factors that can be used to not only see this little miracle at work, but also improve general images.
Back to the Basics of Ultrasound
|
Thermal Index is the heating of tissue as ultrasound is absorbed by tissue, measured by ratio of power used to produce a temperature increase of 1°C. This is measured in soft tissue (TIS), bone (TIB), and in the cranium (TIC). The Mechanical Index is an ultrasound measurement used as estimation of the risk of non thermal effects and the degree of bio-effects a given set of ultrasound parameters will induce; Higher MI means a larger bio-effect. These can include cavitation, the formation of transient or stable bubbles, which can damage tissues. The current Federal Drug Administration has set the maximum MI at 1.9 MI = PNP Peak Negative Pressure of the ultrasound wave |
Before a specific organ, for example the fetal heart, image can be improved on, first obtain the best image possible. To begin any ultrasound study, but especially in Obstetrical scanning, the correct manufacturer’s Preset must be selected. Presets are essentially a “recipe” set for the ultrasound system. These parameters may include depth, gain, frequency, and focus among other factors. Using the OB Preset sets the Thermal Index (TI) and Mechanical Index (MI) which are generally lower for obstetric ultrasound examinations. In general, the TI and MI are not deliberately manipulated during routine ultrasound examinations.
Which Knobs Can Improve Your Picture?
Once the Preset is selected, consider the overall gain in the image on the monitor. Is it all black, all white, or a combination with many grays? Adjust the overall gain, often a large dial easily accessible, so it is easiest to identify the landmarks and in general is appealing to one’s eye and interpretation. This may differ somewhat with each sonographer, but not to an extreme.
The importance of correctly interpreting the landmarks cannot be over stressed, know the anatomy well.
Be sure the size of your image, or depth, allow demonstration of the area of interest. On some machines, this is either a dial knob or toggle switch labeled Depth, Size, or a combination of these. There is a scale on either side of the image that registers this depth in either centimeters or millimeters, and changes as the dial/toggle is adjusted.
Most transducers/probes are multi-herz, which means they offer more than one frequency, usually 2, 4, and 6 MHz. Once the landmarks have been identified and the overall gain is satisfactory, try each frequency with a simple adjustment and determine which provides the best penetration and resolution.
Remember:
- The lower the frequency, the higher the penetration but lower the resolution.
- The higher the frequency, the less the penetration but the better the resolution.
This means images of a patient with Large Maternal Body Habitus (LMBH) most often improves with the lowest frequency, and our smaller, more athletic patients can use the higher frequency for better resolution images. The frequency is often displayed at the top of the image where the TI and MI are located.
The optimal area of the ultrasound beam is the focus, demonstrated by a triangle or karat along the depth scale. Place this at the area of interest at the correct depth. On some systems, the focus makes a significant difference in clarity, but in other systems, there does not appear to be much change.
After the above have been set to optimize the image, the slide pods or TGC/STC can be used to fine tune the image even more. These are a step alteration in the gain, with the slides on the top affecting the top of the image and vice versa. Most often the “slope” is a gradual downward slope to the right.
Manufacturers frequently have specific image enhancing features under proprietary names which reduce haze, clutter, and artifacts allowing for improved clarity of images. These harmonic features may allow for increased penetration without details lost. Simply turning this feature on and determining its benefit (or not) is required.
Looking at the Heart
Once the optimal image has been achieved by using the features discussed above, there are additional tips to see that small fetal heart.
Some systems have a Field of View (FOV) which has the effect of “coning down” and creating a smaller field visible and increases image clarification. This is the consequence of taking only a portion of the available area to scan instead of the entire area seen prior to using this option. Often, a pie-shaped icon is on the image top to illustrate and highlight the FOV area.
Using the Zoom option will increase the image size, which also can make it easier to visualize the fetal heart. In addition, most of the Zoom also has a feature which allows the size of the area, or box, to be increased/decreased. Another key to using a zoom option is to be certain the item of interest is directly in the center of the box.
When viewing the small fetal heart, another gain adjustment making the image brighter aids in recognizing the wave form during Motion-mode (M-mode). This gain is sometimes located by turning the M-mode dial. The brighter the image, the more likely the wave form is visualized. Also, the wave form will be in direct relationship to the location of the heart in the 2 Dimensional (2 D) image. For example, if the heart is in the center, the q, r, s, etc. waves will be in the center of the strip. If the heart is at the bottom of the image, the wave form will be at the bottom of the strip.
Oftentimes, maternal respirations interfere with achieving a well demonstrated strip. To overcome this, ask the patient/client to suspend breathing or hold her breath. Be aware, if she takes in a deep breath, the fetal heart may move out of the image, and you will need to make the necessary adjustments.
All of these discussed options to improve ultrasound images pertain to both Transabdominal and Transvaginal imaging. However, it is reasonable to anticipate that Transvaginal images will be larger and therefore improve the ability to obtain a fetal heart rate.
Using these tips should increase the skill set and confidence for the nurse sonographer and show this little miracle to his or her maximum potential. The tips prior to the “M-mode” can be used for general imaging as well.